Elevating patient voices at EFIC World Congress 2025
Blog by Niamh Walsh
From 24 to 26 April, I attended the 14th EFIC World Congress in Lyon, France as a board member of Chronic Pain Ireland. The annual 3-day Congress brings the latest in pain management and research to 3,500 healthcare professionals and researchers from all over the world. I was excited to see a strong Irish presence with many speakers, chairs, panellists and poster presenters from Ireland.

Pictured at EFIC World Congress 2025 is Niamh Walsh, Chronic Pain Ireland, and Julie Sugrue, University of Limerick.
Mental health theme
The organisers – the European Pain Federation (EFIC) – chose mental health as the focus for this year’s Congress. The theme “Comorbidity of Chronic Pain and Mental Health
Disorders: Breaking the Cycle†highlights the complex connection between chronic pain and mental health. This relationship flows in both directions – mental health issues worsen
chronic pain, and chronic pain worsens mental health conditions.
It’s remarkable just how common mental health issues are with one out of every two people developing a mental health disorder at some point in their life (Kessler et al., 2023). The
Congress emphasised the close relationship between chronic pain and mental health issues highlighting the need for chronic pain treatment to incorporate psychological support.

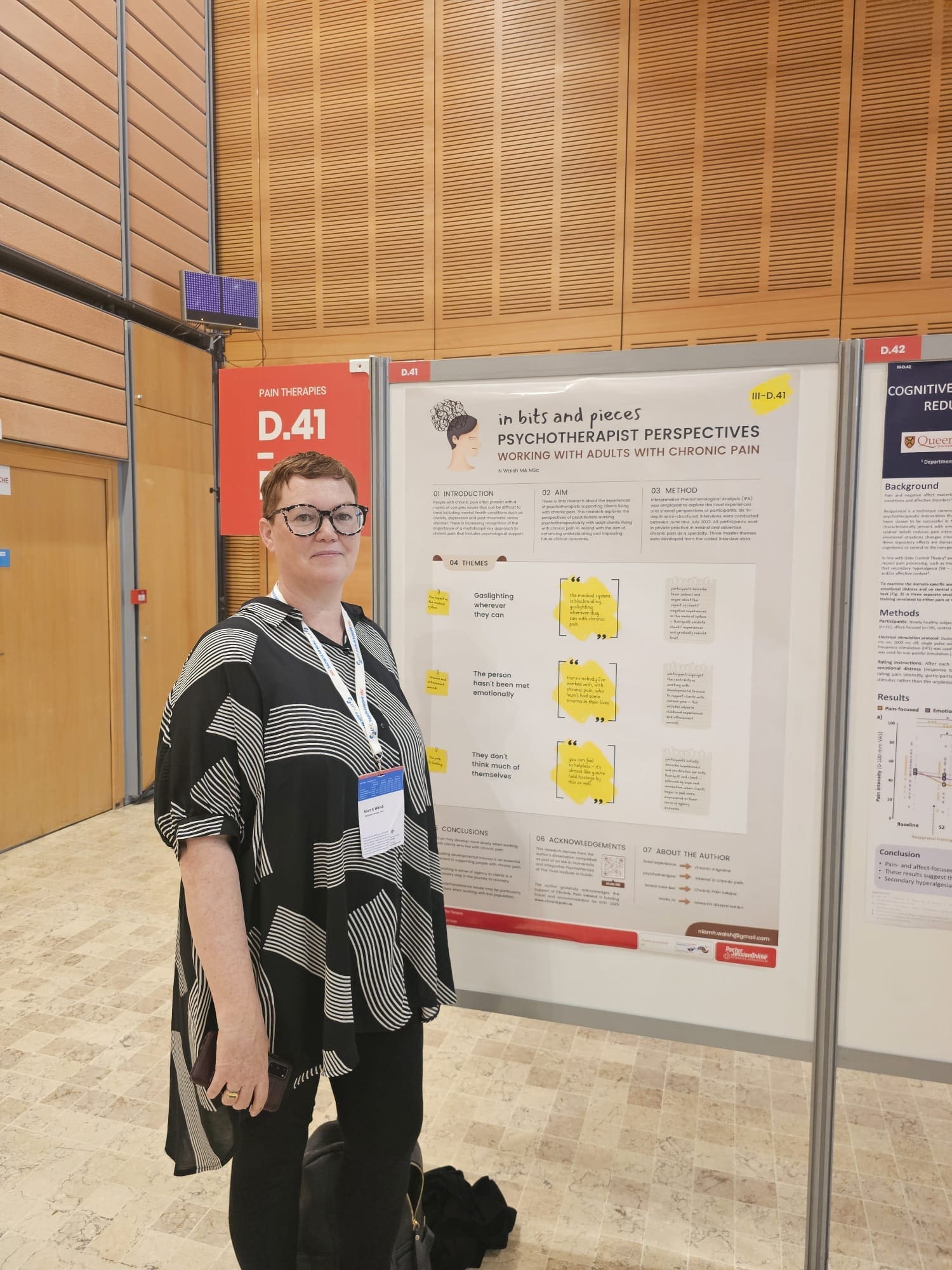
Pictured at EFIC World Congress 2025 is Niamh Walsh, Chronic Pain Ireland, with her poster on the perspectives of psychotherapists who support adults with chronic pain.
Presenting my research
Alongside spending time listening to some fascinating speakers and meeting people from all over the world, I was privileged to present my own research in a poster presentation on the third day of the Congress. My research explored the experiences of psychotherapists working with individuals living with chronic pain in private practice in Ireland.
The anxiety of choice There are multiple streams going on at any one time at the Congress and choosing an option between plenary sessions, masterclasses, workshops, debates and poster presentations can be overwhelming. There were several times I really wanted to attend multiple sessions that were on at the same time. This anxiety of choice was a strong indicator of the excellence and relevance of the Congress programming.
Connecting with people living with pain
While I really enjoyed the sessions and networking, I had to intentionally take breaks and time outs to ensure I didn’t become too depleted. Recognising and accepting the limits of my energy has been a big part of my personal recovery from chronic migraine.
Because it was a pain conference, I got to talk to several people from Ireland and elsewhere who also have lived experienced of chronic pain and understood the need to pause and re-energise when needed. These moments of connection with other people who understand what it’s like to live with pain were the experiences at the Congress that I valued the most.

Pictured at EFIC World Congress 2025 is Niamh Walsh, Chronic Pain Ireland (centre) with Brian McGuire (l) and Rachel Fitzpatrick (r), University College Galway. Professor McGuire is the new SIP Ireland representative along with Niamh Walsh.
Societal Impact of Pain (SIP)
As one of two Irish representatives of the Societal Impact of Pain (SIP) platform, I also joined a valuable SIP meeting and lecture during the Congress. SIP, co-led by the European Pain
Federation (EFIC) and Pain Alliance Europe (PAE) is an initiative focused on policy advocacy to improve quality of life for the 150 million people in Europe living with chronic pain.
Takeaways from the Congress
As a patient representative, these were some of the key insights I took from the sessions I attended at EFIC 2025:
The strong connection between mental health and chronic pain Many sessions emphasised the link between mental health conditions (such as depression, anxiety and trauma) and chronic pain.
I was interested to hear how adverse childhood experiences (ACE’s) and intergenerational trauma can shape a person’s future experiences of pain (Kapos et al., 2024).
Conversely, the experience of chronic pain can lead to anxiety and depression and may be viewed itself as a trauma.
Breaking out of the cycle of experiencing chronic pain and mental health difficulties requires education of patients and clinicians alike and a focus on making trauma-informed care
available to patients. The importance of understanding the biopsychosocial model of pain Effective pain treatment must acknowledge the psychological and social dimensions of pain
– not just the physical.
The importance of understanding the biopsychosocial model of pain
Effective pain treatment must acknowledge the psychological and social dimensions of pain – not just the physical.
The SIP talk ‘Pain and Mental Health: Can Healthcare Professionals and Patients Have a Societal Impact?’ emphasised the need for treatment to consider biological factors (nervous system changes, inflammation, genetics), psychological factors (stress, anxiety, depression), and social factors (employment, stigma, economic conditions).
This means an integrated system of care is critical. SIP argues that a multidisciplinary approach is not sufficient – it’s an interdisciplinary approach with teams working together to support a patient that can lead to optimal outcomes.
SIP have produced a very helpful infographic of the biopsychosocial model of pain.
The critical need for patient inclusion and empowerment
Patients are not just passive participants in their care – they are the experts in their own lives. Shared decision-making, where patient goals and preferences guide treatment plans, leads to greater satisfaction and improved outcomes.
Several sessions stressed the need to define treatment success based on what truly matters to patients and to acknowledge the importance of lived experience in clinical research.
With chronic pain responsible for 50% of work absences in Europe, according to the European Patients’ Forum (2021), the Congress reinforced the urgent need to focus on how we, as a society, effectively address chronic pain.
By supporting Chronic Pain Ireland, you help us advocate for integrated care to ensure that every person living with chronic pain in Ireland is heard and believed – and receives the treatment and care we deserve.
Visit chronicpain.ie to learn more about our services
References
Kessler, R. C., Petukhova, M., Sampson, N. A., Zaslavsky, A. M., & Wittchen, H.-U. (2023).
Lifetime prevalence and age-of-onset distributions of mental disorders in the World Health Organizations World Mental Health Survey Initiative. The Lancet Psychiatry, 10(7), 611–622. https://doi.org/10.1016/S2215-0366(23)00193-1
European Patients’ Forum. (2021). Recommendations for employers: Supporting people with chronic conditions in the workplace. https://www.eu- patient.eu/globalassets/policy/employment/recommendations-for-employers.pdf